Passive and active immunity: what’s the difference and why your body needs both
- READING TIME 5 MIN
- PUBLISHED February 16, 2024
- AUTHOR Donna
Key takeaways
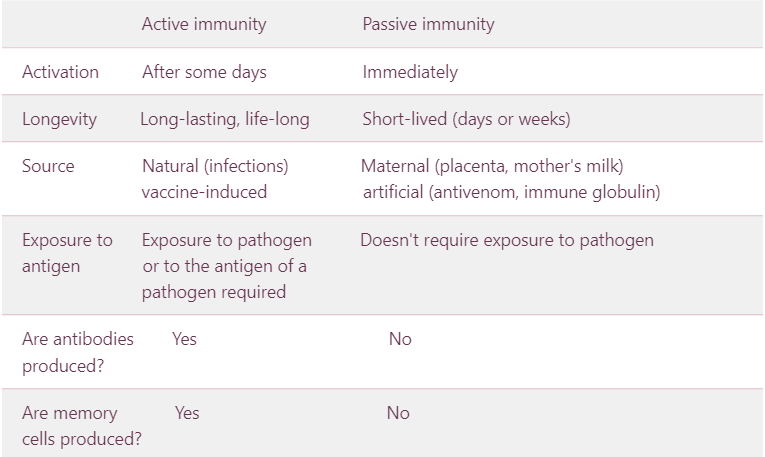
- Active and passive immunity are both critical building blocks of a well-equipped and strong immune system.
- They both use antibodies to neutralize hostile organisms or toxins, but they differ in how the antibodies are created.
- Active immunity is strengthened after an illness or vaccination, while passive immunity depends on receiving antibodies from the outside into the body, for example, from mothers milk, antivenom or blood products like immunoglobulin.
Passive and active immunity: what’s the difference and why your body needs both
Immunity guards your body against pathogens, toxins and other hostile substances which may cause disease or infection. It’s a complex apparatus with different but complementing defensive mechanisms.
Generally, immunity consists of two main systems. One is innate, also known as genetic immunity because it’s inherited or based on genetics. This type of immunity provides protection from birth until death. Innate immunity is made up of physical barriers, such as skin and mucous membranes, saliva or the eye’s cornea. These barriers protect against germs, parasites or cells.1
The second system of immunity is adaptive or acquired, which protects your body against specific types of pathogens. Adaptive immunity is further divided into two types: active and passive immunity. Passive immunity means that antibodies are produced outside the body and introduced into the body. Active immunity, on the other hand, occurs when antibodies are created in the body.2 Both are essential and can keep you safe. Let’s unpack how they work more in detail.

Active immunity: can provide life-lasting protection
Active immunity stems from exposure to a pathogen or antigen of a pathogen. Antigens are proteins that are found on the surface of the pathogen. We are exposed to pathogens everywhere we go – they’re in the air, food and on the surfaces we touch. Most contacts won’t result in an infection, though, either because the pathogen is harmless or your immune system neutralizes the danger without any noticeable symptoms.
Once we get in contact with the antigen, our body starts producing antibodies. These are proteins capable of binding to antigens. Antibodies are specific to a particular antigen – if the body detects the mumps virus, it starts producing antibodies that will only help against mumps and not, for example, against measles or a cold.
We build active immunity in two ways. Firstly, after we recover from exposure to the disease organism or through infection with the actual disease. This gives rise to a natural active immune response usually leading to lifelong protection.3
Secondly, resistance to diseases can also be strengthened by immunization. Vaccines provide us with the possibility to create an immune response in a controlled way. They are designed to not cause illness, which means we benefit from exposure without the risks associated with fighting off a natural infection.4
Either way, if an immune person is exposed to the same disease in the future, their immune system will recognise it and immediately produce the antibodies needed to fight it. This is thanks to the presence of memory cells. These cells circulate at low levels in our bodies. Once they recognize the pathogen in their travels, they quickly start to multiply and signal other elements of the immune system to activate as well.5
Active immunity lasts a long time. While it varies between individuals and diseases, it can endure for years or the entire life.6
Passive immunity: immediately activated, but short-lived
In comparison to active immunity, its passive variation doesn’t require exposure to an infectious agent or its antigen. Passive immunity is built up by receiving antibodies rather than producing them through your own immune system. And while active immunity can take days or weeks to get going (especially after contact with a previously unknown pathogen), passive immunity is activated and can respond against an infection almost immediately.7
Passive immunity can also be natural or artificial. The process of acquiring passive immunity already starts in the womb when a baby receives antibodies through the placenta. After birth, breast milk serves as the key conduit for antibodies, which help to safeguard an infant against certain infections.
Particularly important is the breast milk supplied in the first days after birth known as colostrum which is very rich in protein. This kind of natural (also called maternal) passive immunity is crucial until the baby develops a strong immune system on its own.8
Artificial passive immunity, on the other hand, typically involves injecting a serum with antibodies. One example is getting a shot of antivenom following a snake bite. The same type of immunity is acquired through blood products such as immunoglobulin. The vaccine provides immediate protection in cases of antibody deficiencies such as thrombocytopenia, which is a result of low thrombocyte count.9, 10

Passive immunity is typically only effective for a few days or weeks, far less than active immunity. The reason for a relatively short lifespan of passive immunity is that antibodies are not being resupplied as they are with active immunity where the antibodies are being generated by your own immune system.11
To learn more about how immunity works and how to make sure it performs in top gear, visit our all-encompassing guide.
REFERENCES
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/the-immune-system
- https://www.ncbi.nlm.nih.gov/books/NBK279396/
- https://academic.oup.com/occmed/article/57/8/552/1474357
- https://www.cdc.gov/vaccines/vac-gen/immunity-types.htm
- https://www.chop.edu/centers-programs/vaccine-education-center/human-immune-system/types-immunity
- https://www.nature.com/articles/nm917
- https://www.cdc.gov/vaccines/vac-gen/immunity-types.htm
- https://www.nhs.uk/common-health-questions/childrens-health/how-long-do-babies-carry-their-mothers-immunity/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1809480/
- https://www.mayoclinic.org/diseases-conditions/thrombocytopenia/symptoms-causes/syc-20378293
- https://www.cdc.gov/vaccines/vac-gen/immunity-types.htm
RELATED ARTICLES
Explore more
Feed your curiosity with more content. Dive deeper and explore our selected articles, curated just for you.



