Infertility in women+: causes, treatments and when to see a doctor
- READING TIME 9 MIN
- PUBLISHED November 02, 2023
- AUTHOR Donna
Key takeaways
- The main sign of infertility in women+ is the inability to get pregnant. If you’re not planning a baby, pelvic area pain or unusual menstrual cycles may also indicate infertility.
- The main cause why some women+ can’t get pregnant is a problem with ovulation. Without ovulation, there are no eggs that can be fertilized.
- There are a bunch of methods to investigate infertility in women+, starting with physical examination and blood tests.
- There are also a number of ways how we treat infertility. They depend on the type of the problem, your age and your medical history. The overall likelihood of successful treatment is around 50 percent.
Infertility in women+: causes, treatments and when to see a doctor
Infertility in women+ is diagnosed after one year of unprotected sex that doesn’t result in pregnancy. 1 If you’re older than 35 years, you’re usually entitled to fertility treatment after only six months of baby-making. Female+ fertility declines steadily with age as ovaries become less able to release eggs.
In Europe, around 15 percent of couples experience fertility difficulties. 2 In 30 percent of cases, fertility problems originate in the woman+. The other 60 percent is equally attributed between the man+ or both partners. In around one in ten cases no cause is found, making the cause of infertility ‘unexplained’ or ‘idiopathic’. 3
The main sign of infertility is the inability to get pregnant. But even if you’re not trying to have a baby, you should keep an eye on certain symptoms that may also point to infertility. These signs include pain during sex, very dark or pale menstrual blood, and irregular menstrual cycles with heavy, long or painful periods. 4
How babies are made – a brief explainer
Contrary to popular belief, the odds of getting pregnant are against you in any case. A young fertile couple has one in five chance to conceive in a month. 5
This fertility window (the time when conception can happen) lasts only a couple of days each cycle: 48 hours of ovulation, plus a couple of extra days when sperm can survive in the female+ reproductive tract. You can read more about the fertile window and how you can calculate yours in our article here.

The reproduction process itself is also complex, delicate and doesn’t tolerate any mistakes. 6 So before we look into what can cause infertility, let’s first refresh your “how babies are made” knowledge. This is how it goes:
- An ovary releases a mature egg.
- The egg is picked up by the fallopian tube.
- Sperm swim up the vagina and cervix, through the womb and are propelled into the fallopian tube to reach the egg.
- The fertilized egg travels down the fallopian tube to the uterus. Transport through the tube takes about 30 hours.
- About five to six days after fertilization, the embryo implants itself to the inside of the uterus and grows.
Causes of infertility
The main cause why some women+ can’t get pregnant is a problem with ovulation. Without ovulation, there are no eggs that can be fertilized.
Ovulation occurs when a part of the brain called the pituitary gland secretes hormones that stimulate ovulation. These hormones tell the ovaries to produce follicles and, indirectly, estrogen that works to thicken the uterine wall. All this prepares the body for potential pregnancy. 7
Excessive stress, substantial weight gain or loss can disrupt the production of these hormones, affect ovulation and, with it, the capacity to conceive. 8

The pituitary gland can also cause excess production of prolactin – a hormone that causes breasts to grow and make milk during pregnancy and after birth. Having too much of it can lead to infertility by interrupting or stopping ovulation. 9
Ageing eggs is another significant fertility factor. A woman+ is born with her entire egg supply and, as time passes, these eggs become less effective. The chance of pregnancy for a woman+ aged 40 years is only 5 percent per menstrual cycle. 10
Polycystic ovary syndrome (PCOS) is a common cause of female+ infertility, too. It’s a condition where the ovaries develop many small collections of sacs filled with fluid (follicles). These “sacs” may not release eggs which again hampers ovulation. Women+ experiencing PCOS often have irregular periods or don’t get them at all. 11

The magic of fertilization happens as the sperm meets the egg as it journeys down the fallopian tube. If the road is blocked or scarred, the sperm may have problems getting to the egg or, if it does, the fertilized egg can encounter similar roadblocks getting into the uterus. Previous surgery in the abdomen or pelvis or sexually transmitted infections can cause blockages or damage to the fallopian tubes.
Fibroids (these are non-malignant tumours inside the womb) or overgrowths of the uterine lining may also hamper the implantation of the egg into the uterus. They are found in five to ten percent of infertile women+. 12 Fibroids, which are more likely to negatively affect fertility, grow in the uterine cavity and are larger than 6 centimetres. 13
Another reason that can cause infertility is endometriosis – a condition where the tissue, similar to the tissue that lines the inside of the uterus, grows outside of the womb. It can damage the fallopian tubes and the ovaries and prevent an egg and sperm from uniting. Even if endometriosis doesn’t damage reproductive organs, it can still affect fertilisation, embryo growth and implantation. Estimates suggest that roughly 10 percent of reproductive-aged women+ have endometriosis. 14
In one in ten cases, the cause of infertility is undetermined and can’t be diagnosed. The condition may correct itself with time – but no need to play the waiting game. If you have trouble getting pregnant, discuss the assisted fertility options.
When should you go to the doctor
Speaking of doctors and specialists – it’s recommended that you visit one after a year of unsuccessful baby-making sex. Women+, who are 35 or older, can seek assistance sooner, usually after six months of trying. If you or your partner has a history of fertility problems, you may also have the option to start treatment earlier.
How is infertility diagnosed
There are different methods that healthcare professionals use to investigate infertility in women+. The starting point is the physical examination and blood tests that are used to assess the levels of ovulation hormones. To pinpoint the cause, the infertility doctor may also perform ultrasound scans or take a sample of cervical mucus. This fluid plays fundamental role in the conception process as it nourishes the sperm on its way to the egg.
Another tool doctors use for diagnosing infertility is hysteroscopy. A surgeon will perform the procedure by looking inside of the cervix and uterus using a thin tube. The device is inserted through the vagina and offers a direct view of the uterine cavity. Hysteroscopy can effectively detect intrauterine changes that could interfere with the implantation or growth of the embryo. 15
If these and others fertility tests don’t produce conclusive results, laparoscopy can be used. 16 Laparoscopy is a procedure where a surgeon inserts a telescope-like instrument through a small incision in the tummy. The device is equipped with a light and a small camera that helps the surgeon to examine the pelvis, uterus, fallopian tubes and ovaries for possible blockage, scar tissue or endometriosis.

Treatments: medication, surgery and assisted conception
Although fertility science has come a long way, it doesn’t guarantee pregnancy in any way. The overall likelihood for successful treatment is 50 percent. 17 The success rate of infertility treatments varies greatly, depending on the type of therapy and personal circumstances, most notably age – as years go by, the chances decrease. 18 19
Treatments are most likely to benefit women+ whose infertility is because of problems with ovulation. 20 To help encourage ovaries to release the egg, these women+ are often prescribed different types of medication that help increase or decrease the production of certain hormones. It’s important to keep in mind that the response to these medications can be unpredictable. 21

Surgery can also help treat certain underlying conditions, such as blocked or scarred fallopian tubes, and to remove uterine fibroids, polyps or patches of endometriosis. In fact – if endometriosis is minimal or mild, surgery can double the chances of pregnancy. 22
If medications or surgery don’t help, many couples decide on assisted conception. The type of assistance depends on the causes of infertility, age and possible history of previous pregnancies.
Around one in four in-vitro fertilisation treatment (IVF) cycles, for example, now results in a baby being born. The cumulative effect of three full cycles increases the chances of a successful pregnancy to 45–53 percent. 23
IVF is only one in a number of assisted fertility options women+ have at their disposal. Here’s the rundown:
- Intrauterine insemination (IUI): sperm is placed directly into the womb at the time of ovulation using a small catheter.
- In vitro fertilisation (IVF): eggs are retrieved from a woman’s+ ovaries and fertilized with sperm in a laboratory dish. The embryos are transplanted into the womb or can be frozen for future use.
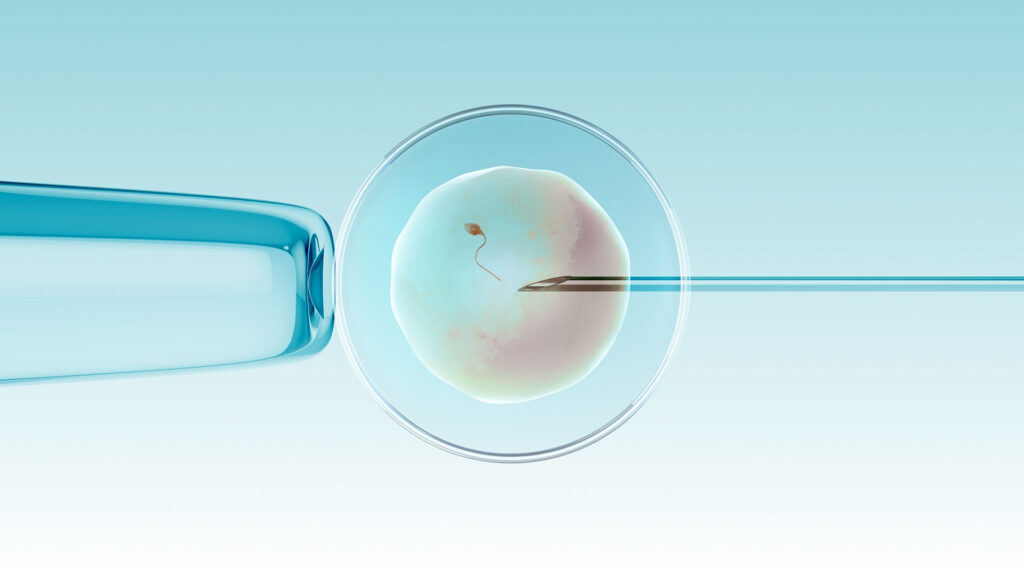
- Intracytoplasmic sperm injection (ICSI): somewhat similar process as IVF but in the case of ICSI, a selected sperm is injected directly into the egg in the lab. The embryo is then transplanted into the womb.
- Donated sperm: donor sperm is either injected into the uterus or used to fertilize eggs in the lab. This method is used if the man+ has a low sperm count or produces no sperm at all.
- Donated eggs: eggs of another woman+ can be combined with your partner’s sperm. The resulting embryo is then implanted in your womb.
- Surrogacy: another woman+ carries the baby to term. The embryo can also be donated.
Prevention – what can you do today
Unfortunately, not much can be done to prevent infertility that is caused by genetics. But in some cases, you can take steps to potentially increase the chances of conception and a healthy pregnancy. 24
Firstly, avoid heavy drinking and smoking. They both negatively affect fertility capabilities. Overweight and underweight women+ are at increased risk of ovulation disorders. Paradoxically, too much exercise is also not good. Strenuous, intense exercise of more than five hours a week has been associated with decreased ovulation. Equally important, protect yourself from sexually transmitted diseases. sup>25
And we can’t stress this enough – go see your gynecologist, have regular check-ups and voice concern if something doesn’t feel right.
REFERENCES
- https://pubmed.ncbi.nlm.nih.gov/29555319/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4424520/#CR11
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/infertility-in-women
- https://www.medicalnewstoday.com/articles/323401#signs-of-infertility-in-women
- https://www.asrm.org/resources/patient-resources/google-adwords-landing-pages/waiting-to-have-a-baby/
- https://www.ucsfhealth.org/education/conception-how-it-works
- https://www.thewomens.org.au/health-information/fertility-information/getting-pregnant/ovulation-and-conception
- https://www.nih.gov/news-events/news-releases/nih-study-indicates-stress-may-delay-women-getting-pregnant
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3461927/
- https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/age-and-fertility/
- https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/
- https://www.fertilityanswers.com/wp-content/uploads/2016/04/fibroids-and-fertility.pdf
- https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/causes/causes-female#f12
- https://www.who.int/news-room/fact-sheets/detail/endometriosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3016139/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5816239/
- https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/treatments/treatments-women#f1
- https://pubmed.ncbi.nlm.nih.gov/22738098/
- https://pubmed.ncbi.nlm.nih.gov/16471151/
- https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/treatments/treatments-women#f1
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/infertility-in-women
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4498168/
- https://www.nice.org.uk/news/blog/the-importance-of-3-full-cycles-of-ivf
- https://www.mayoclinic.org/diseases-conditions/female-infertility/symptoms-causes/syc-20354308
- https://americanpregnancy.org/pregnancy-complications/stds-and-pregnancy/
